Ageism
Like many others, Roslyn Green, at 78 years of age, has been starved and mistreated at the hands of ageism.
“I feel invisible, alone and ignored,” Roslyn said.
“It’s humiliating,” she said.
“Age discrimination has, essentially, starved me.”
For the past seven years, Roslyn has had recurring problems with her esophagus.
She has trouble swallowing and is only able to eat incredibly tiny portions; typically a lunch or dinner will consist of only about three mouthfuls of soft foods. The pain makes anything more completely unbearable.
She had attended several general practitioners in her local Sydney area several times without any result.
“They always told me that it was nothing… just minor inflammation,” Roslyn said.
“They would prescribe me some pain killers and said it should pass… but it never did,” she says.
“Whenever I walked into my doctor’s office I felt like he was just thinking I was making it all up and his time would be better spent treating someone younger… Someone who actually needed his help, because they seemed to think I didn’t.”
Dr Andrew Georgiou, chairperson of the Health Informatics Society of Australia Aged Care special interest group and Associate Professor and researcher at the University of New South Wales, says this is not an isolated issue.
“It’s much more common than people realise,” says Dr Georgiou.
“Age discrimination is an issue that perpetuates [sic] every facet of our society – it’s incredibly prevalent in medicine … even in aged care facilities and it presents a huge problem in our aging community,” he says.
“There’s a huge and growing population of older people in our community and we need to ensure they are adequately taken of.
“Currently, the health of the aged community – both mental and physical health – is a huge industry.”
Dr Georgiou’s statements are supported by Len Gray, a Professor of geriatric medicine at the University of Queensland and Director of the Centre for Research in Geriatric Medicine.
“Society places greater value on younger people,” says Prof Gray.
“Age discrimination is far too common when the aging population is so large and vulnerable,” he says.
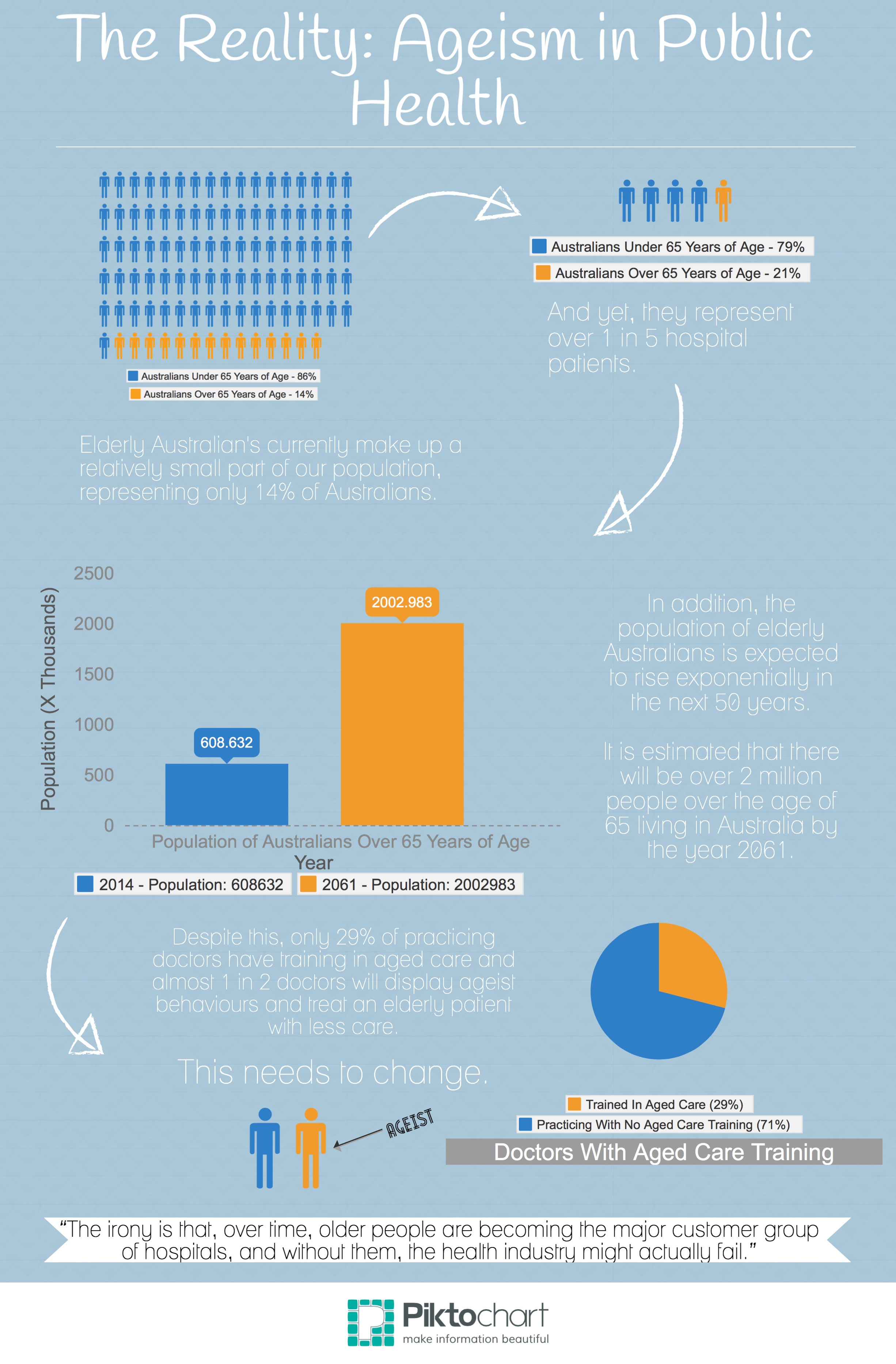
“Over 20-percent of patients attending emergency rooms are elderly persons but our health systems are still often ill-equipped to deliver a suitable standard of care to these patients.
“There’s the idea of ‘a good innings’ that represents the notion that everyone is entitled to a certain amount of life expectancy and quality, and if there are scarce resources, they should be allocated to the people with illnesses who have the most to lose. This approach offers the notion that investment in health should be targeted towards younger people.
“However, much of health care is about symptom relief. In my view, at a minimum, nobody should be in pain, or serious other discomfort, if avoidable.
“Sloppy attention to diagnosis and care is inexcusable at any age.
“The irony is that, over time, older people are becoming the major customer group of hospitals, and without them, the health industry might actually fail.”
However, it still seems that age discrimination is an issue that underlies the reality of the public health sector.
In fact, in recent studies, findings have indicated that nearly half of doctors treated patients with the same symptoms and illnesses over 65 years of age differently to patients less than 65-years-old.
Doctors were less likely to thoroughly test older patients and were more likely to simply adjust their medications and organize a follow up appointment.
Younger patients were more likely to receive detailed testing and access to limited resources such as organ transplants.
This is the same kind of treatment as what Roslyn Green experienced.
Things only changed for Roslyn when she started working with aged care worker, Annette Lee.
“Amongst other things, my job can involve acting as an advocate for my clients during their medical appointments,” says Annette.
“I help them get the care they need and ensure they’re being treated fairly,” she says.
“It’s a service that is sadly becoming an absolute necessity for many individuals.
“When I started working with Roslyn, she had been severely mistreated and her medical needs had been completely ignored.
“She had some terrible issues with her throat and I can’t believe more wasn’t done to resolve the issue.”
Despite her numerous trips to Doctors, Roslyn had been living with an undiagnosed hole in her esophagus for seven years.
When a throat specialist finally diagnosed the hole earlier this year, Roslyn was incredibly frail and weighed only 43 kilograms.
“It’s amazing that she was still in as good health as she was,” says Annette.
“Really, the carelessness of doctors that had treated her in the past could have killed her… they could have starved her to death,” she says.
‘The elderly need to be treated fairly.
“They may have been living longer, but that doesn’t mean they deserve any less.
“There really needs to be a change in this kind of thinking.”
General practitioner, Dr Camilla Ferreira agrees that there needs to be a change in the industry.
“They gloss over it in medical school,” says Dr Ferreira.
“No one ever really emphasized the fact that it’s easy to mistreat elderly patient.”
This is a sad misgiving on the part of the medical industry. Currently, on average, only 29-percent of doctors in hospitals receive training for properly treating elderly patients.
“I hope it can change. It really needs to,” says Dr Ferreira.
“I think that if we simply thought ‘How would I want my grandparents to be treated?’ that we’d see a huge change in the attitudes of the industry,” she said.
If Roslyn Green and the many like her are anything to go by, it is a change that is well overdue.
This post was originally published on Golden-I UQ 2014.
