Suffering in regional Queensland
DALBY resident Scott Doyle was 14-years-old when he passed away from a common bone cancer in March this year. He was one of 10,260 Queenslanders suffering from cancer and living in a regional area.
Scott’s mother, Andrea Bowkett, was forced to move her entire family to Brisbane for 14 months, so that Scott could receive treatment in a city-based hospital where paediatric oncology resources are available.
Ms Bowkett says the financial cost of Scott’s treatment and relocating her family—which also includes three teenage daughters Teagan, Casey, and Lilly—reached over $50,000. The emotional cost is immeasurable.
“The whole family was just turned upside down,” says Ms Bowkett.
“I lost my job, lost my home, and we had to replace all our belongings because they were damaged in storage—it was so overwhelming to think about.
“Of course, my first priority was Scott and his health—I couldn’t leave Scott alone in hospital so Teagan had to look after Lilly most nights; she took on responsibilities that no girl that age should ever have to take on,” she said.
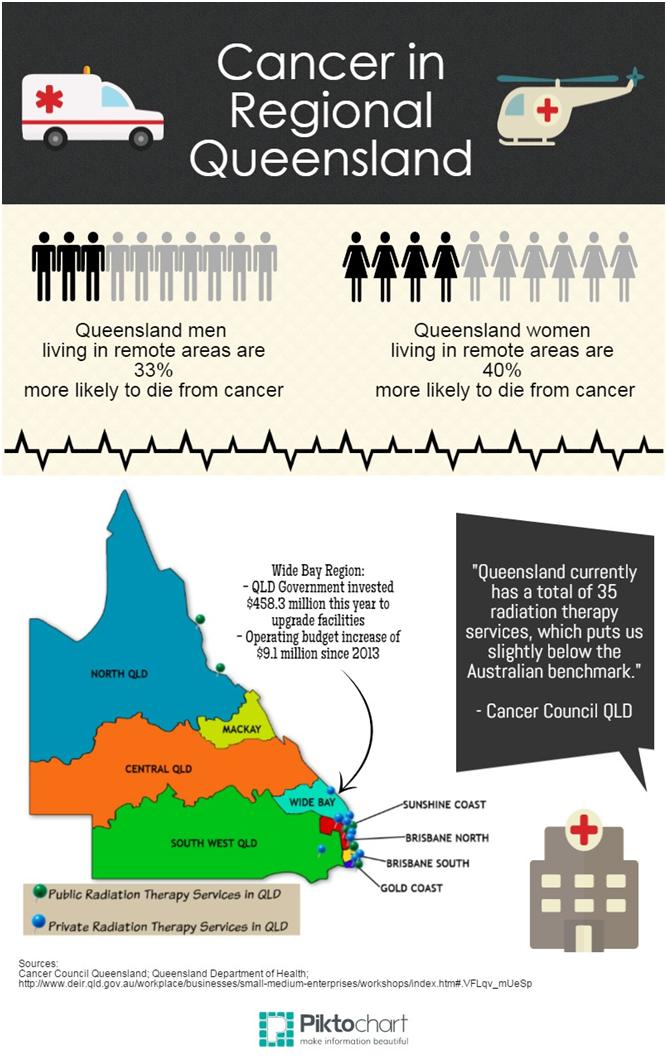
Katie Clift from Cancer Council Queensland says that more than 9% of regional cancer-related deaths could be prevented if regional cancer survival rates were equal to the Queensland average.
“Evidence suggests that the distance to treatment is a barrier for regional cancer patients.
“There are a range of reasons for the cancer death rate being higher in rural and remote areas, such as differences in the management of individual patients, reduced access to health care and diagnostic or screening services, and differences in cancer risk factors such as smoking, diet, alcohol consumption and physical activity,” says Ms Clift.
Lisa Godier, General Manager of Childhood Cancer Support (CCS), says that public oncology treatment needs to be more accessible in regional areas.
“It’s a common misconception that childhood cancer treatments can be accessed anywhere,” says Ms Godier.
“The majority of CCS families have come to Brisbane from regional Queensland, northern New South Wales and the Northern Territory to access cancer treatment for their child.
“This move has far reaching effects on the whole family in terms of their emotional support, relationships, careers, education, mortgages, and pets—the divorce rate is extremely high,” she said.
When Scott arrived at Dalby Hospital, he was diagnosed with an unspecified tumour in his left humerus and was told he would need to travel to Brisbane for further tests with a paediatric oncology specialist.
Those tests revealed Scott was suffering from osteosarcoma and Andrea was told they would need to stay in Brisbane for at least 6 to 12 months.
Andrea and her family managed to stay in free oncology-specific accommodation provided by Childhood Cancer Support, but she has had little financial help.
It took 12 months for her to receive a Carer’s Pension from Centrelink and throughout Scott’s treatment she was expected to look for jobs, which she found impossible given the numerous hospital visits each week.
Dr Shaun Rudd, President of the Australian Medical Association Queensland, agrees that providing oncology-specific services closer to home needs to be a goal for Queensland.
“Increasing oncology services in the regions can be done if the appropriate resources are put into place,” says Dr Rudd.
“There also needs to be support services to complement any such treatments, such as well-trained staff with a case load to make the services cost-effective.
“None of these should be major barriers and depending on the remoteness, different levels of service can be deployed,” he said.
A spokesperson for the Queensland Government Department of Health says that $458.3 million of the 2014-15 state budget has been invested toward the Wide Bay Hospital and Health Service (WBHHS) in regional Queensland so they can provide radiation therapy for cancer sufferers locally.
“The WBHHS partnership with Oceana Oncology provides local radiation therapy to cancer patients with less complex care needs, ending their need to travel to Brisbane,” says the spokesperson.
“Advances in clinical practice enable safer types of chemotherapy to be delivered in district, rural and community health facilities with specialist supervision via telehealth.”
“Cancer patients living in more rural or disadvantaged areas have lower survival rates compared to the Queensland average, but thanks to the growing uptake of telehealth across the state, more rural and remote Queenslanders are receiving specialist medical services,” they said.
Telehealth is not the only remote-access service receiving increased funding.
Sarah Riseley from the Royal Flying Doctors Service (RFDS), which transported 11,125 regional patients this year, says that the Queensland Government has increased funding to cover the increase of regional access points, airstrips, and inter-hospital transfers (IHT).
“In the last five years, the RFDS has experienced an average increase of 4.4 per cent per year in IHT,” says Ms Riseley.
But Andrew Bowkett believes there is a desperate need for more oncology-specific medical support in regional hospitals.
“We need more oncology-trained doctors, nurses, and liaisons in regional areas who know how to handle these (specialist) cases,” says Ms Bowkett.
“Communication between urban and regional hospitals is also extremely important—regional hospitals also need to be more aware of the risks and effects of oncology-related treatments so that regional patients can spend some time at home.”
“Being in home is the best medicine for the kids; it lifts their spirits and actually makes their treatment work more effectively so their health actually improves,” she said.
Ms Clift from Cancer Council Queensland says that regional people can do three things to prevent cancer.
“Firstly, reduce lifestyle risks and participate in screening, secondly, don’t let distance be a barrier to immediately seeing a GP if symptoms arise, and thirdly, comply with treatment recommendations,” says Ms Clift.
Andrea agrees that early detection is important.
“It’s been such a horrific, traumatic experience, but every day, I’m looking at the positives and sharing Scott’s story to help other families that are going through the same thing.”
People who need information, advice, referrals, or practical assistance can contact Cancer Council Queensland’s Helpline on 13 11 20.
Written by Sophie Volker.
This post was originally published on Golden-I UQ 2014.

